
Stem cell therapy is very appealing in its intuitive simplicity: you clean the damaged cells trigger instead a gang of healthy, sit back and wait until the body will not should repair itself. In the case of spinal cord injury the promise of stem cells to restore mobility promises fantastic prospects. However, the human body is not a machine and not a simple system that allows you to replace parts on the fly. After transplantation stem cells are often rejected, dying in the hostile environment of the host organism even before you get a chance to recover.
Over the past thirty years neuroscientists have tried a lot of ways, I tried the cocktail with a cocktail from the special molecules that can accelerate the survival of stem cells. Although models with rodents has been a huge success, scale this therapy to work with primates and it is important for human trials to not work.
Or did not work. Last month in the journal Nature Medicine published an “important” study that detailed the recipe of transplantation of human stem cells that survived and integrated into the damaged spines of monkeys.
Nine months later, after surgery cells dismissed hundreds of thousands of branches that formed synapses with the surviving neurons of the spinal cord of monkeys. Furthermore, spinal neurons of carriers acknowledged human cells as their own and formed new compounds that restored the animal’s ability to grab objects.
“The growth we observed in these cells, the impressive, ten years ago I would have thought it impossible,” says lead author Dr. mark Tushino from the transplantation Institute of neuroscience, University of California at San Diego. “We definitely have confidence that this treatment will work for people.”
Early work
Spinal cord injury cuts the long, thin neuronal branches — the axons — which the brain uses to communicate with the rest of the body. To restore motor function, scientists need to convince the body to repair or grow these connections.
But here’s the problem. After damage to the spinal cord quickly reorganizes the extracellular matrix is a complex network of structural molecules around the injury site. Like the “bricks” on the road, these proteins effectively inhibit transplanted stem cells from stretching their long branches axenovich. Moreover, the injury also deprived of the support of growth factors and other molecules that act as a nourishing cocoon for stem cells.
To work around this double protection, the researchers formed dozens of provoking the growth of cocktails, which could give a boost transplantirovannam cells. And this strategy apparently worked.
In 2014 Tushino transformed skin cells from a healthy donor, of a person, transformed them into cells and iPSC (induced pluripotent stem cells) and implemented these artificial stem cells in a matrix containing growth factors.
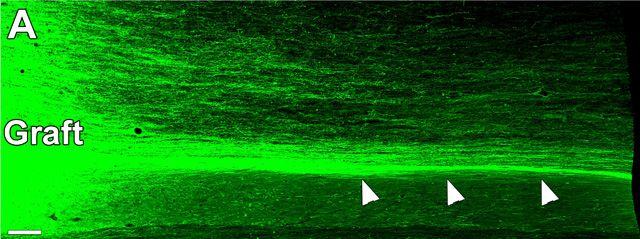
After placement of graft two rats with two-week spinal injuries, human cells matured in new neurons and extended axons in the spinal cord of rats. But strangely, scientists have not seen any improvement functions partly because of the scarring at the transplantation site.
“We’re trying to do everything possible to determine the best transfer method methods of treatment involving neural stem cells in patients with spinal cord injury,” said Tushino at the time.
New hope
True to his word, Tushin experienced your Protocol transfer in monkeys that are better suited as a model for the spinal cord of man.
The team crashed into a section of the spinal cord of a monkey and two weeks is sufficient time for patients stabilized — introduced human stem cells into the damaged area along with growth factors.
Didn’t work. The first four monkeys introduction not even locked in place.
“If we tried to transplant on humans without prior animal testing, and would be a significant risk of failure in clinical trials,” said Tushin.
Scientists quickly realized that they need to increase the number of important protein ingredient in your recipe to better to attach the graft in place. The team also found problems with the immunosuppression, timing and surgical procedure. For example, they had to tilt the surgical table during surgery, to the cerebrospinal fluid is not washed away the graft. In addition, the monkeys needed high dose of immunosuppressive drugs to the body is not attacked human cells.
Using some lotions grafts, each of which contained about 20 million stem cells, held in place by the remaining five monkeys.
The results were incredible. Just two months after the transplantation, the scientists found an explosion of new neural branches. Stem cells at the injury site developed to Mature neurons, spread to 150 000 axons, which stretch in the spinal cord of monkeys.
Some of the branches were at a distance of 50 mm from the graft, of approximately the length of the two spinal fragments in humans. Along the way, they established extensive contacts with intact cells of monkeys.
What’s even more cool, self axons of the apes also formed synapses with neural graft of a human, forming a reciprocal relationship. These connections are very important for free movements of the hands of people and this is one of the first clear evidence that transplanted stem cells can form such schemes.
Nine months later, when new neural connections helped monkeys with damage to regain movement in their limbs so that they were able to grab soft objects (e.g., oranges). In contrast, monkeys with poor grafts poorly controlled precise movement in hands and fingers — could only push orange.
The results may seem not very impressive, but the authors say that nine months is the moment for functional recovery.
“The grafts and the new scheme, part of which they were yet matured to the end of our observations, so the recovery can continue,” said study author Dr. Ephron Rosenzweig.
Hot functional improvement was only partial, Dr. Gregoire Curtain from the Swiss Federal Institute of technology (EPFL) in Geneva, calls the study “a milestone in regenerative medicine”.
“And this is not surprising, given that the functional integration of new cells and connections in the nervous system will take time and specific rehabilitation procedures,” he said, adding that the study offers valuable information for potential human exploration.
Agree with him and Dr. Steve Goldman from the University of Rochester:
“It’s a big jump from rodents to primates. This is a heroic study, if it comes to that”.
For Tushino work is just beginning. First, not all stem cells are created equal, and his team is trying to determine which ones are most effective in restoring function.
On the other hand, it is also exploring additional ways to further enhance the functionality of the regenerated neurons, so that their axons can be spread through the damaged area and replace those that were lost during the injury.
“It is too early to go to the people,” he warns, because further testing required. And this patience will pay off.
Human stem cells are returned to the monkeys the ability to grab objects
Ilya Hel