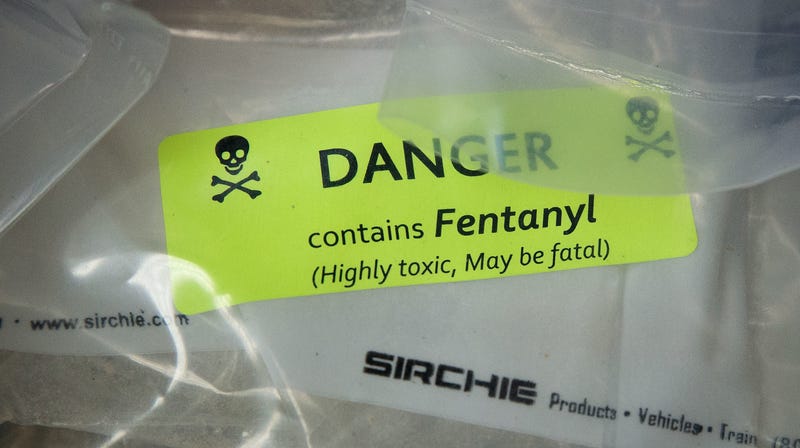
 A sample of heroin laced with fentanyl, collected during a drug bust in New York City in September 2016.Photo: Drew Angerer (Getty Images)
A sample of heroin laced with fentanyl, collected during a drug bust in New York City in September 2016.Photo: Drew Angerer (Getty Images)
More people are dying from drug overdoses in the U.S. than ever before, according to a new preliminary report released Wednesday by the federal government. There were an estimated 72,287 drug overdose deaths last year, the report found, with the majority caused by opioids. The toll is yet another record high.
The report is only an provisional estimate of reported overdose deaths, since some reported deaths still haven’t been fully investigated. But the final tally is unlikely to be off by much. Compared to the 63,000 overdose-related deaths seen in 2016, there was roughly a 10 percent jump in only one year. Of these 2017 deaths, more than 60,000 involved opioids, though some deaths may have been caused by more than one drug.
“These data are devastating, and further underscore the need for an all-hands-on-deck approach from health systems and communities to provide compassionate, evidence based care,” Honora Englander, an assistant professor of medicine at Oregon Health & Science University, told Gizmodo. “This is not a moral failing or a choice. It’s a ruthlessly painful condition.”
The new figures aren’t surprising to opioid policy experts such as Leo Beletsky, an associate professor of law and health sciences at Northeastern University.
“They indicate that, in many places around the U.S., the response continues to miss the mark.” Beletsky told Gizmodo via email.
Indeed, the overdose-related death rate increased across most of the country, with states such as New Jersey, Nebraska, and North Carolina reporting the largest increases. Only 11 states, including Vermont, Wyoming, and Montana, reported a lower overdose-related death rate in 2017 than in the year prior. In terms of raw numbers alone, both Florida and California saw more than 5,000 overdose deaths last year.
The report seems to confirm the changing shape of the opioid crisis, now driven by potent synthetic opioids such as fentanyl. Nearly 30,000 deaths were attributed to fentanyl in 2017, an astonishingly dramatic rise from the less than 5,000 deaths recorded annually prior to 2014.
Fentanyl, which can be up to 50 times more potent than heroin, has become a major source of the illicit opioid supply in the country in the past few years. Usually shipped from overseas, the drug is cheaper to produce and transport than other street opioids. While some users purposefully seek out fentanyl, oftentimes dealers discreetly cut their advertised heroin products with the drug. Users might then overdose because they take more of what they mistakenly believe is a weaker strength opioid. Aside from being deadlier, there’s even some research suggesting the drug can also cause other unique health problems, such as amnesia and cognitive damage.
Despite the sobering findings, Englander says there are well-established but often ignored ways to help people struggling with addiction and prevent deaths.
“We know that people with opioid use disorder who receive treatment with medications like buprenorphine and methadone have dramatically reduced mortality and yet nationally there remains a massive shortage of treatment providers, payers often don’t cover these life-saving medications, people are denied access to treatment while incarcerated, and there remains tremendous stigma which interferes with people’s well being and interest in treatment,” she said.
Englander herself has helped build a novel program at her university’s affiliated hospital that connects willing hospitalized patients living with opioid use disorder to social workers and dedicated specialists.
“We need to build systems that include the voices of people who are suffering from opioid use disorder,” she added. “Including them at the policy and treatment level is so important.”
While the current Trump administration has called—inconsistently—for greater substance use treatment access, it’s also sought policy changes that many opioid experts and patient advocates have criticized as self-defeating and harmful to chronic pain patients.
The Centers for Medicare and Medicaid Services, for instance, has pushed for strict prescribing restrictions to be forced onto Medicare patients. These would require insurers to deny payment for opioid doses over a certain daily amount, as well as prevent new patients from being prescribed an initial treatment course longer than seven days. In Oregon, even stricter restrictions are being floated, such as mandating that all long-term opioid therapy be cut off by 2020 for Medicaid patients.
Critics have argued that these proposals will not only do little to deter opioid use disorder, since most prescription opioid users do not develop addiction, but may actually cause some otherwise stable pain patients to spiral out of control and seek more dangerous opioids illicitly. Others might become heavily depressed and suicidal.
“I think the folks who put this together didn’t do so willy-nilly, but there’s not really evidence supporting it,” said Englander of the Oregon plan. “We really need to be cautious about a blanket approach.”
Given the small successes seen driving down the mortality rate in some states, there is room for optimism, Beletsky said. But only if we embrace what works.
“Unless we double down on increasing access to the antidote naloxone, rapidly scale-up evidence-based treatment, and address the underlying health and other needs of people who use drugs, the destruction wrought by this crisis is going to continue surging,” he said.
[CDC via The New York Times]